A pacemaker, also called a cardiac stimulator or a battery, is an electronic device designed to regulate the heart’s electrical activity, which is essential for effective contraction.
This small device consists of two main parts:
- The generator, which houses the electronic circuits and a battery, producing the necessary electrical impulses.
- The leads, conductive wires that transmit electrical impulses between the heart and the generator to synchronize the heartbeat.
For more information: What is a pacemaker?

When Pacemaker Installation is Necessary
A pacemaker is indicated for patients suffering from certain heart rhythm disorders.
Its implantation can occur in two contexts:
- Short hospitalization: When correcting the heart’s electrical activity is urgent.
- Scheduled intervention: In non-urgent cases, the procedure can be performed on an outpatient basis, by appointment.
Scheduling the Appointment
When the installation of a pacemaker is recommended, the physician submits a request to a qualified institution to arrange the procedure.

Pre-admission Meeting
The hospital then contacts the patient to schedule a preparatory meeting before the procedure, which is typically performed as a day surgery.
During this meeting, it is essential to bring an up-to-date list of all medications the patient is taking.
The Day of the Procedure
Reception and Preparation
On the day of the procedure, the patient is welcomed by the medical team responsible for preparation. It is imperative to fast starting at midnight the night before.
Medication
The patient must strictly follow medical instructions regarding their usual medications.
Some treatments, particularly anticoagulants, must be stopped the day before or the day of the procedure. If unsure, it is preferable not to take the medication and inform the medical team upon arrival at the hospital.

Updating Medical Records
A brief questionnaire is completed to update medical information, including known allergies.
Physical Preparation
The patient changes into a hospital gown. A nurse places one or two intravenous lines to allow for the administration of saline or medications, if necessary, during the procedure.
Hospitalization
In some cases, the patient may need to remain at the hospital until the next morning for observation.
Consent Form
After being informed of the risks associated with the procedure, the patient must sign a consent form. These risks are detailed later in this text.
At this stage, the physician has determined that the benefits of the procedure outweigh the risks.

Procedure Risks
Before proceeding with pacemaker implantation, the physician carefully weighs the benefits and risks to ensure this intervention is the best option for the patient.
Although pacemaker implantation is generally safe, like any medical procedure, it does carry certain risks.
Risk of Death
The risk of death associated with this procedure is extremely rare, estimated at less than 1 in 1000 cases.
Major Complications
The risk of major complications, estimated at 5–7%, includes issues that may require correction during or after the procedure.
These complications can occur either during the procedure or in the days and weeks following it.
–Complications During Pacemaker Installation:
- Pneumothorax: This may occur if the needle used to puncture the subclavian vein accidentally perforates the lung lining, causing air leakage into the chest cavity.
- Significant Bleeding: Hemorrhage requiring immediate intervention may occur during the procedure.
- Pericardial Effusion: Bleeding in the membrane surrounding the heart can result from an electrode accidentally perforating the right ventricle.
-Complications Following Implantation:
- Infection: Occurs at the incision site or around the pacemaker device.
- Hematoma: BloodBlood is composed of red blood cells, white blood cells, platelets, and plasma. Red blood cells are responsible for transporting oxygen and carbon dioxide. White blood cells make up our immune defense system. Platelets contribute to blood accumulation at the procedure site.
- Electrode Displacement: When one of the leads shifts and loses proper contact with the heart, which can disrupt stimulation.
- Thrombosis: Vein obstruction caused by leads inserted into the subclavian vein.

These risks, while real, are managed by an experienced medical team. Precautions such as administering prophylactic antibiotics and closely monitoring the patient post-procedure are implemented to minimize these outcomes.
Each patient is informed of the specific risks prior to the procedure, and measures are taken to ensure that the benefits far outweigh the risks.
Final preparatory steps
When the time comes, the patient is taken to the procedure room. Before starting, antibiotics are administered through the pre-inserted venous catheter to prevent any infection related to the procedure.
Once these preparatory steps are completed, the medical team proceeds with the intervention, ensuring the patient returns to the same room for the recovery phase after the operation.
Entering the Room
The patient is welcomed by a specialized team that assists them in transferring from the stretcher to the examination table.

The procedure room, resembling an operating room, may appear impressive. The staff wears sterile equipment, such as masks, surgical caps, and lead aprons, to protect themselves from the X-rays used during the intervention.
The ambient temperature, intentionally cool, ensures the proper functioning of medical equipment.
To provide comfort and ease any anxiety, sedation is administered through the venous catheter already in place.
The patient’s upper body is uncovered, and electrodes are placed on various parts of the skin to monitor cardiac activity.

The pacemaker is typically implanted in the upper left part of the chest.
A generous application of antiseptic liquid, often cold, is used to disinfect the area. This liquid may cause a temporary sensation of cold or warmth, especially in men who have had prior chest shaving.

After disinfection, a sterile drape is placed over the patient’s chest to minimize the risk of infection.
At this stage, it is essential for the patient to remain still for the duration of the procedure.
Anesthesia
The implantation of a pacemaker does not require general anesthesia.
Local anesthesia is used to numb the targeted area, ensuring the procedure is painless while keeping the patient awake.
The Procedure Itself
The implantation of a pacemaker is a relatively simple and generally well-tolerated procedure. A small incision is made in the chest, usually on the left side, to create a pocket under the skin that will house the pacemaker’s generator.

Through this incision, the physician locates and punctures the subclavian vein, which allows for the introduction of one or more leads, also called electrodes, connected to the generator.
These leads are guided to the heart using radiological imaging (X-rays) to ensure their precise positioning and proper functionality.
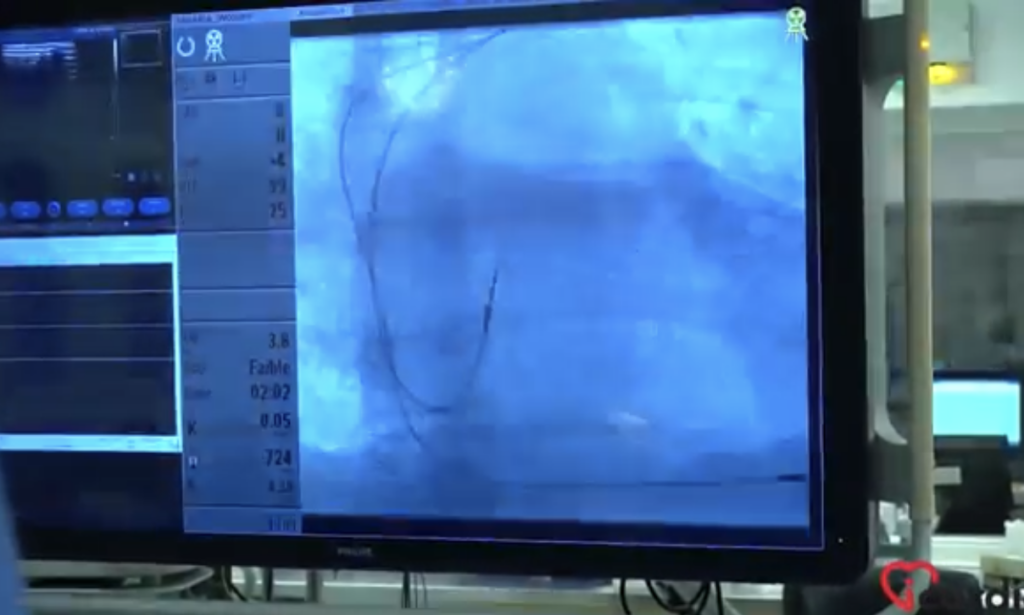
Once the electrodes are in place and their function validated, the skin pocket is closed using dissolvable sutures. These absorbable stitches naturally dissolve within a few days following the procedure, eliminating the need for manual removal.
Return to the Preparation Room and Monitoring
After the procedure, the patient is brought back to the preparation room where they were welcomed earlier in the day. A monitoring period is then initiated to assess their general condition and ensure the proper functioning of the newly implanted pacemaker.
This phase is crucial for the prompt detection of any potential complications, such as bleeding at the incision site or issues with the device’s operation.
The length of monitoring varies depending on the health center’s protocols and the patient’s overall health status.

In some cases, patients may be discharged the same day, while others may require extended observation until the following morning.
Upon Patient Discharge
Before leaving the hospital, the patient is provided with an information sheet containing essential details about the implanted pacemaker. This document includes the technical specifications of the device, its serial number, and the manufacturer’s name.
A few days after returning home, a plastic card with the same information will be mailed to the patient. This card is useful for medical follow-ups and for informing healthcare professionals during future consultations or procedures. It is recommended to keep it with you at all times.
What Happens at Home?
Before leaving the hospital, the patient receives written instructions detailing the necessary care, monitoring, and precautions to take in the days following the procedure.
This document is essential, as patients often forget some of the verbal advice given by the medical team.
The key points addressed include:
- care for the incision site,
- warning signs that should prompt a medical consultation,
- activities to temporarily avoid,
- myths and facts regarding living with a pacemaker.
For more information, see: Living with a New Pacemaker.

After a short recovery period, most patients can resume a normal life, with minor adjustments based on medical recommendations.
Pacemaker or Cardiac Device Follow-Up
A first appointment at a specialized clinic is usually scheduled within 1 to 2 months after the implantation. During this visit, a doctor or healthcare professional examines the incision site to ensure proper healing and verifies the pacemaker’s functionality using a specialized programming device.
This follow-up also provides an opportunity for the patient to ask questions about the use and maintenance of their pacemaker. The medical team ensures that any adjustments made to the device are explained clearly and offers advice to optimize its use.
These regular check-ups are essential to ensure the device functions properly and to guarantee the patient’s safety, while also addressing any concerns they may have.

Pacemaker or Cardiac Device Follow-Up Procedures
The follow-up of a pacemaker can be carried out in two main ways: through visits to specialized clinics or remotely via telemonitoring technologies.
• Follow-Up in Specialized Clinics
The most common method involves attending a specialized cardiac device clinic once or twice a year.
During these appointments, the pacemaker is assessed to ensure it is functioning correctly, and any necessary adjustments are made. These visits also provide an opportunity to evaluate the patient’s overall condition and address any concerns they may have.
To learn more: Pacemaker Clinic
• Remote Monitoring
Remote monitoring offers a practical and efficient alternative. Using a wireless device installed at home, often placed in the bedroom, pacemaker data is transmitted automatically and regularly to a specialized center.
This type of monitoring can sometimes detect abnormalities or changes in device performance earlier than scheduled visits.
It is particularly beneficial for patients living far from specialized clinics or those who wish to avoid travel, especially during difficult weather conditions. Additionally, it provides extra peace of mind through continuous and proactive surveillance.

Transmission of Results to the Referring Physician
The results of the pacemaker implantation are sent directly to the physician who initially requested the procedure.
Requesting a Copy for Another Physician
If another healthcare professional, such as your family doctor or a different specialist, needs to be informed about the procedure, it is important to specify this. Otherwise, these physicians will not automatically receive a copy of the report.
To have the results sent to them, simply provide the medical staff with the name and contact information of the relevant physician. This request can be made at any time, either before or after the procedure.