We often hear about people who suddenly collapse, sometimes with no known illness. In many of these cases, the heart suddenly stops functioning, leaving no time to intervene.
Sudden cardiac death occurs when the heart abruptly stops pumping bloodBlood is composed of red blood cells, white blood cells, platelets, and plasma. Red blood cells are responsible for transporting oxygen and carbon dioxide. White blood cells make up our immune defense system. Platelets contribute to blood, often due to a severe arrhythmia. This leads to a sudden loss of consciousness, respiratory arrest, and, in the absence of immediate resuscitation, death.
Most of the time, there are no warning signs. However, some people may experience chest pain, palpitations“Palpitation” is a symptom related to an abnormality in heartbeats. There are several types of arrhythmias. This term is like a surname that encompasses several first names., or dizziness in the minutes or hours before the event.

How big is the problem?
An estimated 32,000 people die from sudden cardiac arrest each year in Canada. These deaths may account for half of all cardiac-related deaths, making it the leading cause of mortality—ahead of heart attacks, cancer, and strokes.
In the United States, the numbers are even more striking: more than 350,000 deaths per year, most occurring outside the hospital. That’s nearly 1,000 deaths per day.
Who is affected?
Sudden cardiac death mainly affects adults aged 30 to 50. Men are affected twice as often as women. In children, it remains rare, with about 1 to 2 cases per 100,000 per year.
Among young individuals, cardiac arrest often happens during team sports (around 1 in 200,000 athletes).
Among people over age 35, it occurs more frequently during individual sports like running or jogging—about 1 in 50,000 marathon runners and 1 in 15,000 joggers.
What causes sudden cardiac death?
The immediate cause is almost always a serious arrhythmia, particularly ventricular fibrillation. But this electrical disturbance is usually related to underlying heart conditions, which differ by age.
In people over 40, the most frequent cause is coronary arteryThe two coronary arteries, the right and the left, form the blood network that supplies the heart with oxygen and nutrients. They are located directly on the surface of the heart and branch into smaller vessels that disease. It can go unnoticed before the event, making sudden cardiac death difficult to predict.
In younger individuals, the cause is often a congenital abnormality—present from birth—that affects the heart’s structure or electrical system.
What is the difference between sudden cardiac arrest and a heart attack?
Sudden cardiac death is not the same as a heart attack. The heart is a muscle whose role is to pump bloodBlood is composed of red blood cells, white blood cells, platelets, and plasma. Red blood cells are responsible for transporting oxygen and carbon dioxide. White blood cells make up our immune defense system. Platelets contribute to blood throughout the body. This pumping action is coordinated by an electrical system that triggers regular, organized contractions.
In a heart attack (myocardial infarction), one or more coronary arteriesThe two coronary arteries, the right and the left, form the blood network that supplies the heart with oxygen and nutrients. They are located directly on the surface of the heart and branch into smaller vessels that become blocked, reducing oxygen to part of the heart muscle. This damages the tissue, but the heart usually continues to beat.
In contrast, sudden cardiac death is caused by an electrical failure, most often ventricular fibrillation, during which the ventricles lose all coordination. BloodBlood is composed of red blood cells, white blood cells, platelets, and plasma. Red blood cells are responsible for transporting oxygen and carbon dioxide. White blood cells make up our immune defense system. Platelets contribute to blood flow stops, and without it, the brain shuts down quickly, causing loss of consciousness, respiratory arrest, and eventually death—unless prompt action is taken through CPR and defibrillation.
What are the symptoms?
In more than half of all cases, there are no symptoms before cardiac arrest. The event is totally unpredictable.
However, some people may feel chest pain, palpitations“Palpitation” is a symptom related to an abnormality in heartbeats. There are several types of arrhythmias. This term is like a surname that encompasses several first names., or dizziness, followed by a sudden loss of consciousness.
What are the risk factors?
Several factors can increase the risk of sudden cardiac death. Some are linked to known heart diseases, while others may go unnoticed until the event occurs.
The two main risk factors, found in the majority of victims, are:
- a history of heart attack (in about 75% of cases);
- coronary arteryThe two coronary arteries, the right and the left, form the blood network that supplies the heart with oxygen and nutrients. They are located directly on the surface of the heart and branch into smaller vessels that disease caused by atherosclerosis (in more than 80% of cases).
Other contributing factors include:
- a left ventricular ejection fraction below 40%;
- a history of heart failure (increases risk eightfold compared to the general population);
- a family history of sudden cardiac death;
- long QT syndrome;
- Wolff-Parkinson-White syndrome (pre-excitation due to accessory pathway);
- unexplained syncope;
- a family history of syncope or cardiac arrest;
- congenital heart defects;
- dilated or hypertrophic cardiomyopathy;
- obesity;
- diabetes;
- and drug use that may disrupt heart rhythm.
How is the diagnosis made?
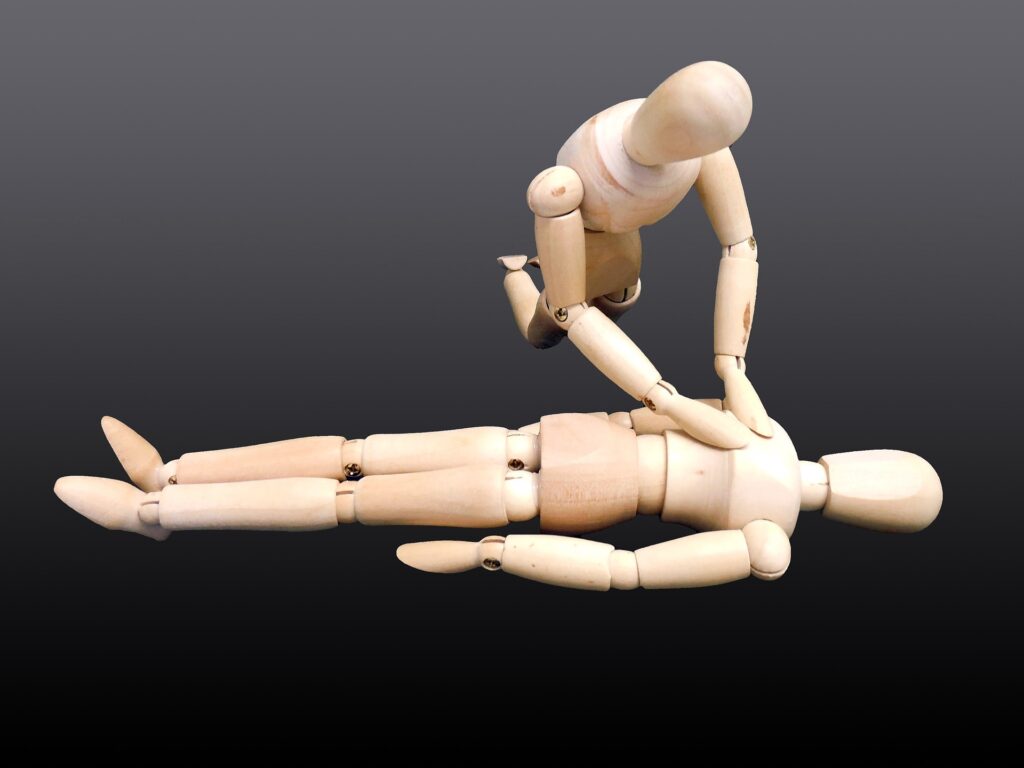
A person who collapses suddenly, loses consciousness, and is unresponsive may be in cardiac arrest. CPR should be started immediately, and 911 must be called.
If an automated external defibrillator (AED) is available, it should be used as quickly as possible.
Recommended reading: Automated External Defibrillator (AED)
Unfortunately, in most cases, victims do not receive help in time and never reach the hospital. They are often found deceased, with no resuscitation attempted.
If the person is successfully resuscitated and transported, the diagnosis is confirmed using an electrocardiogram (ECG) or rhythm strip documenting the arrhythmia. Further testing is then done to identify the underlying cause.
What is the treatment?
In patients who survive the initial event, a coronary angiogram is usually performed quickly to check for blockages that may have triggered the arrhythmia.

Additional tests are conducted during hospitalization to determine the exact cause and prevent recurrence. Treatment may include:
- coronary intervention, if a blockage is present;
- medications to control heart rhythm;
- and often, the implantation of an implantable cardioverter-defibrillator (ICD).
What is an implantable cardioverter-defibrillator (ICD)?
An ICD is a small device placed under the skin, usually in the upper chest, just below the collarbone. It functions like an advanced pacemaker.
In addition to stimulating the heart when it beats too slowly, it can detect and correct dangerous arrhythmias.
If needed, it delivers an electric shock to restore a normal rhythm—potentially saving the person’s life.

What is the prognosis?
Even when resuscitation is successful, the prognosis remains guarded. Most out-of-hospital cardiac arrests are fatal. About 70 to 90% of victims die at the scene. The most favorable statistics—around 70% mortality—are reported where AEDs are available, such as in schools and sports centers.
Among the 10 to 30% who survive the initial arrest, only 5 to 40% leave the hospital alive. Some will recover fully; others will be left with severe neurological impairments.
How can this prognosis be improved?
Rapid and effective resuscitation remains the key factor.
But beyond emergency care, prevention is still the best approach. Being aware of one’s risk factors and adopting heart-healthy habits—such as treating known cardiac conditions, eating well, staying active, and avoiding harmful substances—are all essential to lowering the risk of sudden cardiac death.